It is really easy when something is wrong with you to enter into a spiral of blame and despair.
You can start to blame everything on your illness. *Maybe I have tinitus because people with my disease can have hearing problems.* *All those years I stood in front of speaker stacks dancing in clubs, and the headphones I used to blare on full blast, those things have nothing to do with the ringing in my ears.* *I have a sore hip to I must have hip problems because that’s what is common in people with my disease.* *My sore hip has nothing to do with all the stairs I was climbing last week, I must be falling apart.*
You can start to blame each ache and pain on whatever is wrong with you.
Then you blame your doctors for not getting things right. You blame the health service when they aren’t fixing the woes. *My foot hurts and I need new orthotics but the health service is too slow!* *Maybe stretching and icing can help the pain I’m experiencing until I can be seen by the NHS, but damn the NHS is horrible as I have to wait so long!*
It is easy to despair. To become overwhelmed, and sink into hopelessness. *Nothing is ever going to make me feel better.* *There is no cure for what is wrong with me.*
Or. You can take charge.
I had my epiphany moment a few years ago, the moment when I realised that the way I handled living with CMT was going to be up to me. I decided that in order to stay fit I would need to get fit. I realised that good health was not something I could take for granted, that it was something I would have to work on for the rest of my life. And in my epiphany moment I realised that I – and only I – would be able to assemble and manage the right team to help me to manage my health.
Yep. I realised in order to manage living with a progressive degenerative nerve disease I needed to pull together a support team. A group of experts with whom I connect and who would sign up to my mission – to become as strong as I possibly can, from the inside out, in order to live the best possible life for me.
I’ve been asked recently about the support I receive. Specifically, who I am working with, and for details about the full range of support I have sought out over the years.
Assembling My Team
I have said many times before that I cannot do what I do without the support of a complete team of people – friends, family, doctors, coaches and the like. I don’t think that everyone necessarily needs a team – but when you face challenges or are new to something, I’ve found a team or support group certainly helps.
I am really lucky – I have been able to find people to work with who actively want to help me to achieve my goals. I think this is the key to success – not only am I willing to commit to the pursuit of my own health and fitness, but I have been able to find people who are as excited as I am about helping me to achieve what I set out to do. I know that each person I work with is on my side. How have I done this?
I have a pretty simple rule when it comes to people – I like to make sure I take net positive energy from everyone I engage with. This helps me to stay positive, even when times are tough.
I guess there is only one big rule I have when it comes to my health – and that is that health is not just about being active. I have chosen a total approach, meaning that I pay attention to all aspects of my well being – from food and fitness, to sleep and fun.
My Mental Approach?
What is my mental approach? Simple: be positive. A PMA (positive mental attitude) is what it is all about for me.
Living with a progressive degenerative nerve disease is not about living in despair. Sure – there are moments when I get down. And the down can make me feel low. But the low? It is temporary. Rather than despair, the way that I look at it is that living with CMT has provided me with the chance to get to know the way impacts on me and therefore to better understand my current limitations. And with this understanding, I have chosen to see if I can beat today’s limits. By doing this – facing and beating my limitations – I am developing patience, learning commitment, and I know that I need to be prepared “to fail” knowing that the only true failure is not trying in the first place. Courage, commitment, patience, positivity – I know that I need to build these qualities myself, and also that I want those that I work with to have the same.
I decided to engage with everyone I want on my team in a way so that they know I value them as a part of my solution – as an integral part of my life philosophy. I try to let them know that they are key to how I live with and manage the challenges I experience. I want them to share in my successes and achievements – I don’t just go to them when things go wrong, but I make sure to let them know when things go right. I don’t want to be the number that shows on someone’s phone when I call to cause them to hit the button that sends me to voicemail. Instead, I want the people I work with to feel excited about working with me so that they pick up my calls and help me to achieve whatever my next aim is.
My Team
The Doctors, Physios, and Orthotists Who Make It Happen
When I was diagnosed with CMT in 2004, the last thing I wanted to do was engage with my medical team. I think the appropriate description would be DENIAL. I didn’t want to know what my future could look like, as everything that Dr Google was telling me fit into the category in my mind that was labelled “grim”. But when I decided in 2007 to do my first triathlon, I decided that I would check with doctors to make sure it would be ok. With this decision, I also decided to create positive engagement with my medical team. So that in 2009, when I decided to learn how to run, I also decided that my medical team would be a part of my big support team.
I am a patient at the National Hospital for Neurology and Neurosurgery in the UK, which also includes the Centre for Neuromuscular Diseases (of which CMT is one of many managed and researched). Mary Reilly is one of the foremost CMT researchers in the world and practices at the Centre running a CMT clinic, but I am looked after by Matthew Parton.
There is very little that doctors can actually offer CMT patients, except for regular monitoring and access to interventions (pain medications, physiotherapy, occupational therapy) if required. I see Matthew about once a year for a regular “touch base” appointment, and he has supported me tremendously over the years. His support has included writing a letter disclosing my CMT to my employers, being available for the follow up investigation into the consequences of CMT on my job performance undertaken by my employer following my disclosure, and also Matthew has also provided the medical clearances I require to be able to participate in athletic endeavours. Georgie Mewing, the clinical specialist, fields my many questions and helps me out with appointments that I need, research I am seeking, or any other random requests that I may have (such as when I am able to pick up my orthotics).
As I have a confirmed case of CMT (genetic confirmation of my exact type) I am able to participate in ongoing research studies. Sometimes this is as simple as completing a questionnaire on pain (rare in my case, although I occassionally get electric shock type pain in my hands) or fatigue (I struggle to know what is neural fatigue versus normal fatigue, so found this a tough questionnaire to answer). Other times it has involved working with physiotherapists on exercise interventions into CMT (one particular study took 9 months of committed participation). I like to think of the researchers as a part of “my team”. I engage with them, asking for copies of work that they think I might find interesting.
I have been lucky enough to work with Gita Ramdharry at the Institute of Neurology. Gita is a research neurophysiotherapist, and she practices both for the UK National Health Service as well as privately. I see Gita as a private patient, to fine tune my strength and rehab related to doing triathlon with CMT.
I have also seen others on the physiotherapy team at the National Hospital. In May and June Vicky helped me to also manage some shoulder issues I was developing before the Great Chesapeake Bay Swim. My initial wait for an appointment was about 3 months, and thereafter I was able to be seen for follow up appointments every 2-3 weeks until I was “cleared” from the ongoing case management list.
Finally, orthotics. There is probably nothing more crucial to my day-to-day management of CMT than the condition of my feet. Except for maybe fatigue management (although that is the subject of another blog post for another day!).
Feet are often the first sign of CMT. Here is a diagram of a typical “CMT Foot” (from the Muscular Dystrophy Association).
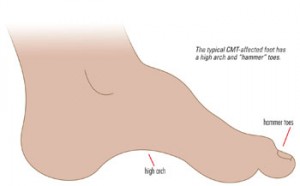
The fact that I received a confirmed diagnosis of CMT initially started because my feet were sore. Management of foot pain, tendonitis, and other issues has been a constant feature in my life with CMT. I have been to countless appointments to make, remake, recast, try and try again to get my orthotic solution perfect. And when I think it may be close, chances are that my feet and muscles have changed again, kicking off the process for yet another round.
I am fortunate to be working with some great orthotists from TruLife, including Elaine Nelson. I have seen Elaine at both the National Hospital and also at the TruLife laboratory near Birmingham in the UK. The opportunity to go to the gait lab was amazing, with proper pressure plate analysis done of my running form, and the next generation solutions made for my orthotic inserts in late 2010. I know that all the work on my run will lead to changes, and that what works today with my orthotics may need to change tomorrow (in fact, I am waiting for the next steps on how to tackle some issues with my right foot). I have a feeling that the quest for good feeling feet is going to be a constant in my life! The “right support” is key to this.
The Coaches
I decided in 2009 that I was going to commit to triathlon, and part of this decision entailed finding a triathlon coach. I met with Terence Collins in August 2009 after my London Triathlon, knowing that I needed help. I wanted to find a coach to work with to develop my running skills, to become a faster swimmer, and to provide and shape a plan to help me to train and mix three sports together into one race while managing CMT.
In June of this year I sought out specialist advice in running biomechanics. People with CMT tend to have certain characteristics such as hip flexor dominance. I knew that in order to be a faster runner, and more competitive paratriathlete, that I would need to re-learn running and work on basic biomechanics. I have been working with James Dunne of Kinetic Revolution since June, to do this. The progress has been incredible, including my first ever treadmill run yesterday (I can’t feel my feet particularly well on a treadmill, but James showed me how to approach things in a safe way so that I could maximise my training in the bad weather months).
I believe that specialist coaching has been really key to my improved performance in triathlon. For example, I knew I needed help on the bike so attended the Strong Like Bull training camp in February. When I have a weakness, I seek out experts to help me to address and manage it.
I realise coaching is not for everyone, but if you are considering it perhaps the questions I ask myself might be of use to you.
The Therapists (of the sports variety)
My muscles can get really tight. Not just the tight associated with doing a lot of activity – but the tight associated with a tendency to atrophy caused by poor nerve transmission and muscle stimulation.
Since 2007 I have been seeing Michael Collins, a sports therapist, for sports massage which includes myofascial release, soft tissue release, neuromuscular stimulation and other therapies to help my muscles to relax, stay supple and healthy while I train. I find sports therapy to be a vital part of my training.
I have also over the years seen specialists for other techniques such as Intramuscular Stimulation (a muscle release which inserts acupuncture needles directly into muscle trigger points to stimulate contraction / release). I don’t seek out IMS regularly but when I do, I see Julie Gear at Physio in the City.
Nutrition
Food and eating healthy (and well) have always been a part of my life. Maybe it’s because when I was little my mother had a garden, and she “made her own” of all of our favourite things (like apple pie – yum! – and pickles). I love food, and really believe in a few approaches, “everything in moderation” as well as “home made is best”.
When I was first diagnosed with CMT in 2004, I sought out the advice of a nutritionist with expertise in using food as a way to manage health and conditions. I have seen Vicki Edgson off and on since 2004, usually going in for a tune-up and the latest advice on eating for neurological health about once or twice a year. I always prepare for our sessions with a list of questions I have, plus I keep a food journal (of my no holds barred eating, like what I posted in August) so that Vicki can see what I have been doing and provide me with tips and advice on how to improve my habits.
In 2010 I also began to work with Christine Lynch, The Holistic Guru, on sports specific nutrition and well being. Working with Christine has been a pleasure – I have been able to pick up so many great lifestyle tips, and she has really given me the tools needed to eat for sport (including race day nutrition).
Is A Good Team Down To Luck?
A comment made to me in a particular context (I admit this is out of context on this post, but it still is an interesting comment) is that not everyone is as lucky as me to have such great support.
I don’t actually think that great support is about luck.
Rather, I think it is about attitude and approach.
When it comes to my health, I try to find experts to work with, people who find my challenges interesting, and I try to be open, communicative and positive when I work with people. It really really helps to get people on your side – whether you are managing illness or seeking to achieve a new goal or dream.
Let’s face it – no one likes to work with a Debbie Downer. This is true when it comes to managing CMT or anything else in our lives. Maybe the lucky thing is that I am naturally a positive person – a skeptic, a truth seeker, a realist, but fundamentally positive.
I hope that by sharing my experiences – whether or not you have CMT – you might find something of value in this post – perhaps something in how I approach doing what I do that you could take into your own life, or maybe a component or individual in my support network could also help you. I think my overall approach – trying to find a TEAM of people to help me to achieve my objectives – is just as applicable for healthy people seeking new challenges as it is for challenged people seeking health.
What are your top tips for getting the right team in place to help you with your challenges?
i think you’re so right about overcoming the mental side and having a good support system. sometimes it can be hard to find those people that will stick with you and push you when you need it most, but it sounds like you have a great team in place. i’m still working on this…
Having just found out that I do indeed have CMT after suspecting it for quite a while, coming across your blog was exactly what I needed to see. Now that I know what is wrong with me I fianally can begin the processing of trating my disease and working with my body after all those years of pushing and doing more harm than good. Thank you for being such an uplifting inspiration!
What a great post on staying upbeat in the face of difficulty and specifically helpful information for anyone who is dealing with CMT or any other health issue.
I especially love, and as I grow older, relate to this:
“I have a pretty simple rule when it comes to people – I like to make sure I take net positive energy from everyone I engage with.”
I think it’s the only way to have a sane life!
Thank you guys so much for the positive feedback. I am glad you find this post helpful – with or without a nerve disease like CMT, I think little things like a PMA can go an awful long way. I am by no means always Susie Sunshine, but I do my best to remind myself how great life is, including *all* of its challenges.
And… Thanks for being a part of my support network!
Donna, I simply love this post, and I wish all my clients could be like you:) I loved you line, about how you don’t want your phone call to be ignored, and you want them to be excited about working with you. What an awesome way to look at things. I always get excited to work with my clients, but there are always those ones, that make it difficult. You have an amazing support network, and your positive energy and attitude rubs off on me:) I love it!
Hi Donna,
I came across your blog while looking for a solution for a nerve disease like CMT, I have now an idea how to treat this and will share this to some of friends who are experiencing this as well. Excellent post.
– Conrad Simone